Calcium is one of the five major minerals of the body. The parathyroid gland, also called the ‘calcium thermostat’ maintains a level of 8.6 to 10.3mg/dL of this mineral in the blood.
Calcium has four critical functions in the body:
Table of Contents
Toggle1. Builds and Protects Bon
The medical and advertisement industries have long pushed for the importance of consuming adequate calcium to maintain good bone health. This is because 99% of calcium is stored in bone tissue while only the remaining 1% circulates in the blood.
When excess calcium is circulating in the blood, a quantity of it is absorbed and deposited in the bone as calcium phosphate salts crystalize and strengthen the bone. Conversely, when blood calcium levels drop, these calcium salts from the bone are released into the bloodstream.
Thus, chronic calcium deficiency can cause the weakening of the bones due to the consistent bone resorption process.
2. Helps Blood Clotting
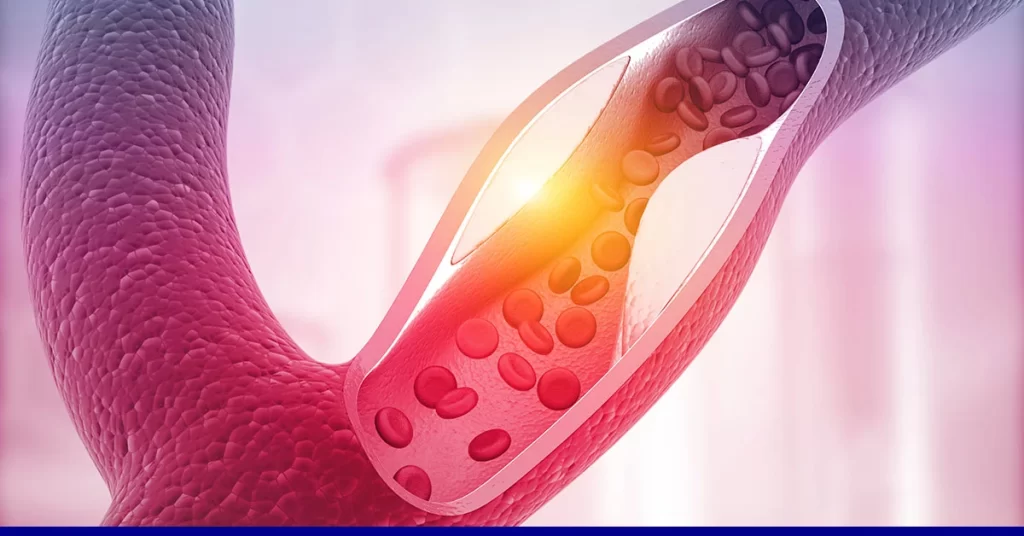
Calcium is one of the key minerals involved in the clotting cascade. When a blood vessel is damaged, it needs to be repaired timely to prevent profuse bleeding, leading to death. Clotting factors and platelets are perpetually circulating in the blood to quickly remedy such instances. However, some clotting factors require calcium for activation – without which the clotting cascade cannot reach completion.
3. Muscle Contraction
Calcium is required to generate and complete a cycle of skeletal muscular contraction. It is required to contract the muscle and also cause muscle relaxation; if the calcium level drops in the cell, the muscle cannot relax. This results in a persistent muscular contraction, causing stiffness and involuntary twitching.
4. Nerve Impulse Transmission
Although calcium itself is not a neurotransmitter, it binds to neurotransmitter vesicles at neuronal synapses and causes their release to carry forward the action potential. In conditions when the body is dangerously deficient in calcium, nerve impulses are not transmitted effectively due to the lack of release of neurotransmitters and results in lethargic motions.
Calcium is a cornerstone mineral of the body and a deficiency can result in weak and brittle bones, lethargy, tetany, and profuse bleeding, as discussed above. However, an excess of calcium may be equally dangerous. A high blood calcium level is indicative of the presence of plaque in your arteries (as plaque contains calcium), which poses several health threats, as discussed below.
What Causes Excess Calcium in Arteries?
It is known that a high intake of calcium in the diet does not cause calcium buildup. So, what causes excess calcium in arteries?
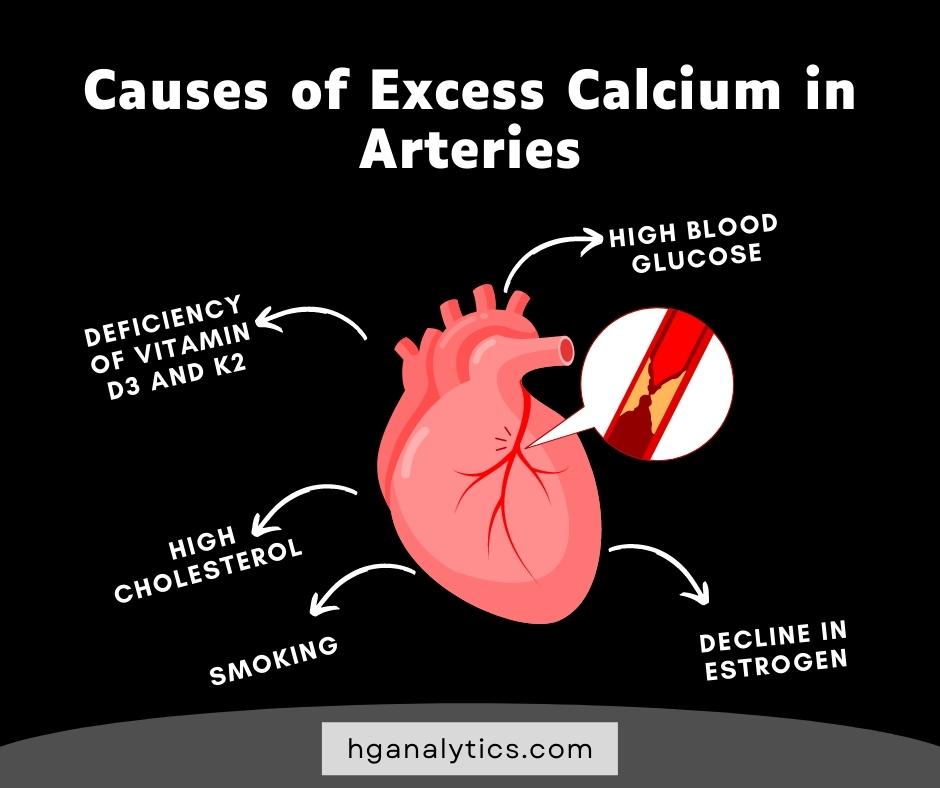
The exact cause is unknown; however, researchers have been able to determine a few factors that contribute to calcium depositions in arteries.
1. Smoking
It has been noted that smokers maintain a higher level of arterial calcium.
2. High body fat percentage and cholesterol intake
The hardened atherosclerotic plaques are mainly composed of fat, cholesterol, and calcium. Thus, high levels of any of these substances in the body increase the chances of plaque formation.
3. High blood glucose
Individuals with diabetes may show high blood glucose levels due to the inefficiency of insulin regulation. High blood glucose damages arterial walls. During the healing process, calcium is deposited in the damaged wall, which may lead to hardening and a loss of elasticity.
4. Deficiency of Vitamin D3 and K2
These vitamins facilitate the absorption and metabolism of calcium in the body. When the body is deficient in vitamins D3 and K2, calcium is not utilized by the body cells effectively and circulates in the bloodstream.
5. A Decline in Estrogen
It has been noted that calcium buildup in arteries begins in a male’s teenage while women mostly undergo calcification of arteries after menopause, once estrogen levels in the body start to drop.
Dangers of Calcium Buildup in Arteries
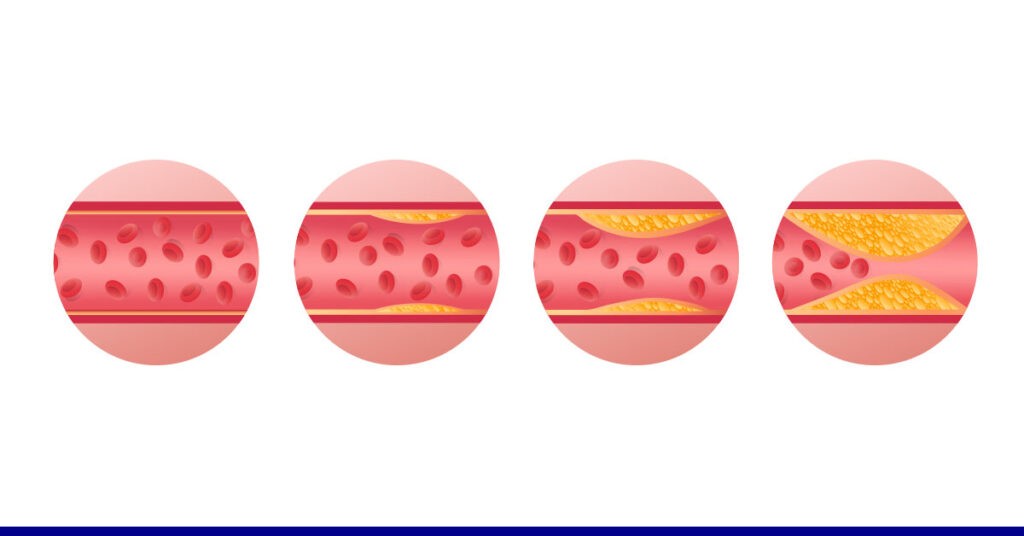
The primary danger posed by excess calcium in arteries is that it can combine with cholesterol to form a plaque, resulting in the hardening of the arterial wall. Loss of elasticity and partial blockage due to the hardened plaque can have devastating effects, ranging from obstruction of blood flow and oxygen supply to a region to a heart attack.
This condition is known as atherosclerosis. It can cause a heart attack, permanent damage to heart tissue, stroke, and severe pain.
Symptoms of Calcium Buildup in Arteries
Symptoms of calcium buildup in an artery only manifest when the plaque begins to obstruct the blood flow to a region.
If the plaque exists in a coronary artery, you may experience:
- Chest pain
- Shortness of breath
- Slow or rapid heartbeat
If the plaque is present in an artery supplying blood to the brain, you may feel:
- Dizzy, difficulty in maintaining balance
- Weakness in the limbs
- Slurring of speech
- Loss of memory
Similarly, if a peripheral artery is blocked, you may feel numbness or tingling in the limbs, or pain in the affected area.
Prevention and Treatment
Consuming a healthy, balanced diet, and regular exercise is the key to preventing most lifestyle-related diseases. Lifestyle changes can prevent coronary calcification and although the condition cannot be reversed, they can slow the progression of the condition is diagnosed. If you want to prevent arterial calcification, you must:
1. Quit Smoking and Alcohol
Smoking gives rise to several life-threatening issues, one of which is the degradation of the inner arterial lining. Plaque cannot collect in the arterial wall the lining is intact and unbroken.
2. Exercise
Exercising regularly and maintaining a healthy weight prevents obesity and lowers the body fat percentage. Burning body fat through cardio and weighted exercises removes fat from the blood quickly, reducing the probability of plaque formation.
3. Consume a Healthy Diet
Your diet should consist of high fiber and low saturated fat content to reduce LDL cholesterol and prevent atherosclerotic plaque buildup. In addition, sodium intake should also be curtailed. Sodium raises arterial blood pressure, which can damage arterial walls over time. This increases susceptibility to calcium buildup in the arteries.
You should regularly take any medication prescribed by your doctor, especially if you suffer from hypertension, hypercholesterolemia, or diabetes since these conditions can expedite plaque formation.
4. Diagnosis
If your doctor suspects calcification of your arteries, a Heart Scan is performed to detect calcium buildup in your coronary arteries and estimate the risk of coronary artery disease. Also called a calcium scoring test, the Heart Scan is a non-invasive test using a CT scan to measure your blood calcium levels.
An understanding of coronary calcium can accurately predict cardiac risk and directly measures blood vessel damage. Your calcium score then helps your physician recommend lifestyle changes or appropriate medication to mitigate the effects of the excess calcium in your arteries.
The Bottom Line
Despite being a keystone mineral in maintaining good health, an excess of calcium in arteries can cause a buildup of the mineral. Combined with vessel damage and high cholesterol levels, excess calcium in arteries can result in dangerous atherosclerotic plaques.
Now that you are aware of the causes of calcium in arteries, you should make the appropriate lifestyle changes to protect your health.
At HG Analytics, we offer top-notch preventative care services to help you identify diseases you may be at high risk for, such as calcium buildup in your arteries.