20-40% of the worldwide population suffers from chest pain at some point in their life. 5% of emergency visits and up to 40% of emergency admissions are due to chest pain complaints. Chest pain can occur due to several reasons and is associated with many complications. Thus, in an emergency setting, it is crucial to assess the condition of the patient, and effectively strategize the treatment plan.
For these two purposes, the HEART score is a highly effective tool. It can help assess acute coronary syndrome (ACS) in the patient, as well as gives an insight into the treatment plan.
Let’s look at what exactly is a HEART score, and how it is interpreted for use.
Table of Contents
ToggleWhat Is The Heart Score?
The HEART score is a chest pain risk classification method for patients in the ER. This means that it aids doctors in estimating the patient’s risk of developing heart disease and identifying the current condition, and further categorizing the pain as low to high risk for cardiac complications.
The final score also helps the doctor strategize whether to admit the patient into supervised care in the hospital or discharge them.
If you find yourself in the ER due to chest pain, the doctor will ask for a heart score.
The score is based on:
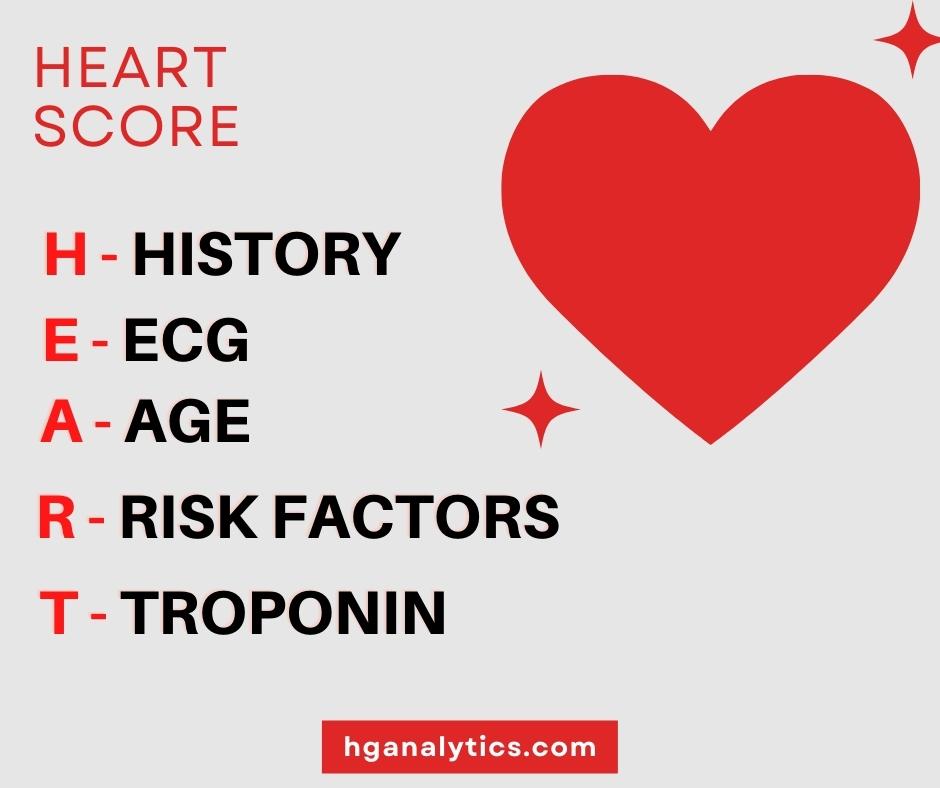
Your doctor may ask you questions and request tests to score each element above on a scale of 0 to 2. The points are added up to give a final score out of 10 that is further interpreted to aid in diagnosis and organizing treatment plans.
Why Is The Heart Score Used?
In an emergency room where thousands of patients are presenting with chest pain, it is important to differentiate and effectively diagnose the small fraction that will be suffering from ACS.
A study showed that when a doctor deals with a patient experiencing chest pain and rules out ischemia as a possible cause, there is still a 9% chance that the patient is suffering from ACS. The formulation of the HEART score method through vigorous studies has helped doctors reach accurate diagnoses.
In patients with ACS, the HEART score helps the doctor calculate the risk for major adverse cardiac events (MACE). MACE is a combination of possible outcomes that consists of myocardial infarction (MI), CABG, revascularization, or death within 30-42 days of presentation of chest pain.
How to Heart Score
In the following segment, each element of the HEART score will be discussed separately in detail. We will also be looking at a patient’s example to illustrate the real-time application of the HEART score.
1. History
A patient’s history may be the most subjective component of the test. So, it is important to carefully gauge the patient’s history before assigning a score.
History that is indicative of cardiac ischemia should score a 2. Such a patient may present with the following symptoms that are specifically associated with cardiac ischemia:
- Left-sided crushing, squeezing, heavy chest pain
- Chest pain that radiates to the left or right arm, shoulders, or jaw
- Chest pain associated with vomiting or sweating
- Chest pain while walking upstairs or on physical exertion
- Chest pain associated with strong emotions
If a patient’s history shows non-specific symptoms, they score a 0. This can look like:
- Right-sided stabbing chest pain
- Chest pain that is reproducible on applying direct pressure, movement, or worse on deep inspiration
- Nausea, shortness of breath
- Non-radiating chest pain
- Chest pain that is short-lasting (less than a minute)
If the patient presents with a combination of specific and non-specific symptoms, then they would score 1 point.
2. ECG
The ECG scores are objective and each score has an associated ECG pattern.
If the ECG has the following characteristics, it should score a 2:
- ST-deviation which may be elevation or depression greater than two millimeters in two contiguous leads
- New T-wave inversion
1 point is given if:
- the ECG shows non-specific or old repolarization disturbance
- The ECG displays a left bundle branch block or hypertrophy of the left ventricle.
0 points are given if the ECG appears to be normal.
3. Age
The scoring of age is straightforward. It is based on cut-off values; the older the patient, the higher the risk.
- Patients older than 65 are given 2 points.
- Patients between 45 and 65 are given 1 point.
- Patients below the age of 45 are scored 0.
4. Risk Factors
Since the HEART score helps identify acute coronary syndrome (ACS), we need to identify the risk factors of the HEART score for atherosclerosis in the patient. The patient is then scored based on the number of risk factors they are vulnerable to.
The risk factors for atherosclerosis include:
- Hypercholesterolemia
- Hypertension
- Positive family history (atherosclerosis in
- Diabetes
- Smoking within the past 90 days. If the patient used to smoke but quit more than 3 months prior, this will not be considered a risk factor.
- Obesity (BMI > 30)
Having an established history of atherosclerotic disease is also highly suggestive of ACS. This includes:
- History of revascularization including procedures like CABG and PCI.
- History of myocardial infarction
- History of ischemic stroke
- History of peripheral artery disease (PAD)
Points are allotted using the following criteria:
- When a patient exhibits any history of atherosclerotic disease OR more than 3 risk factors of atherosclerosis, they are given 2 points on the HEART score.
- The patient scores 1 point when up to two risk factors are applicable.
- 0 points are given when no risk factors are present.
5. Troponin
Like age and ECG, troponin is a straightforward scoring component based on the first troponin measurement in the ED.
- 2 points are given when the troponin is 3x the reference values.
- 1 point is given if troponin levels are between 1 and 3 times the reference values.
- 0 points are given if they are below the reference values.
Interpreting the Heart Score
For patients suffering from chest pain, the HEART score is a tool to quantitatively assess the condition of the patient. Once each component has been scored, the points are tallied to give a final score out of 10.
- A score of 0 to 3 indicates low risk – up to 2% – for MACE. The patient can be discharged safely
- A score of 4 to 6 indicates moderate risk – up to 20%. The patient is usually admitted to the hospital for observation and treatment
- A score above 7 poses a significant risk – up to 50%. The patient must be admitted and early invasive treatment is recommended
What Should Your Heart Score Be?
Ideally, your HEART score should be below 3 to stay within the healthy range. The risk factors for the HEART score are modifiable factors that can be controlled if you lead a healthy lifestyle.
You can prevent and treat heart score risk factors like hypertension, hypercholesterolemia, smoking, and obesity through robust lifestyle changes. Consume a balanced nutritious diet to fuel your body with the resources it needs to function well and quit smoking. Staying active for at least 30 minutes a day and doing cardio exercises have been proven to improve heart health.
If you make the right choices, your risk factors for HEART score can notably decrease, along with lowering your total score and reducing your overall risk for MACE.
If you are interested in preventative care for heart health, HG Analytics can put your health worries to rest by providing top-notch screening tests and identifying any ailments you may have.